The breast is hot and swollen, breastfeeding is becoming more and more painful, and to top it all off, you suffer from fever and aching limbs. It’s not uncommon for breastfeeding mums to show these symptoms during the nursing period, and when they occur, the diagnosis is usually quite clear. It’s mastitis.
Mastitis is a common breastfeeding problem that women experience either during postpartum or at a later stage. In technical language, a breast inflammation that happens while a woman is breastfeeding is referred to as mastitis puerperalis.
Since an inflammation of the breast tissue is quite painful, affected mothers are usually pressed to find out how to treat it. But what causes mastitis in the first place? And is it safe to breastfeed with mastitis?
Table of Contents
What is mastitis?
What does mastitis look and feel like?
How to treat mastitis?
How long does mastitis last?
How to prevent mastitis?
Mastitis vs. clogged milk ducts: What’s the difference?
Will mastitis go away on its own?
Can I still breastfeed with mastitis?
When to seek professional help to treat mastitis?
What is mastitis?
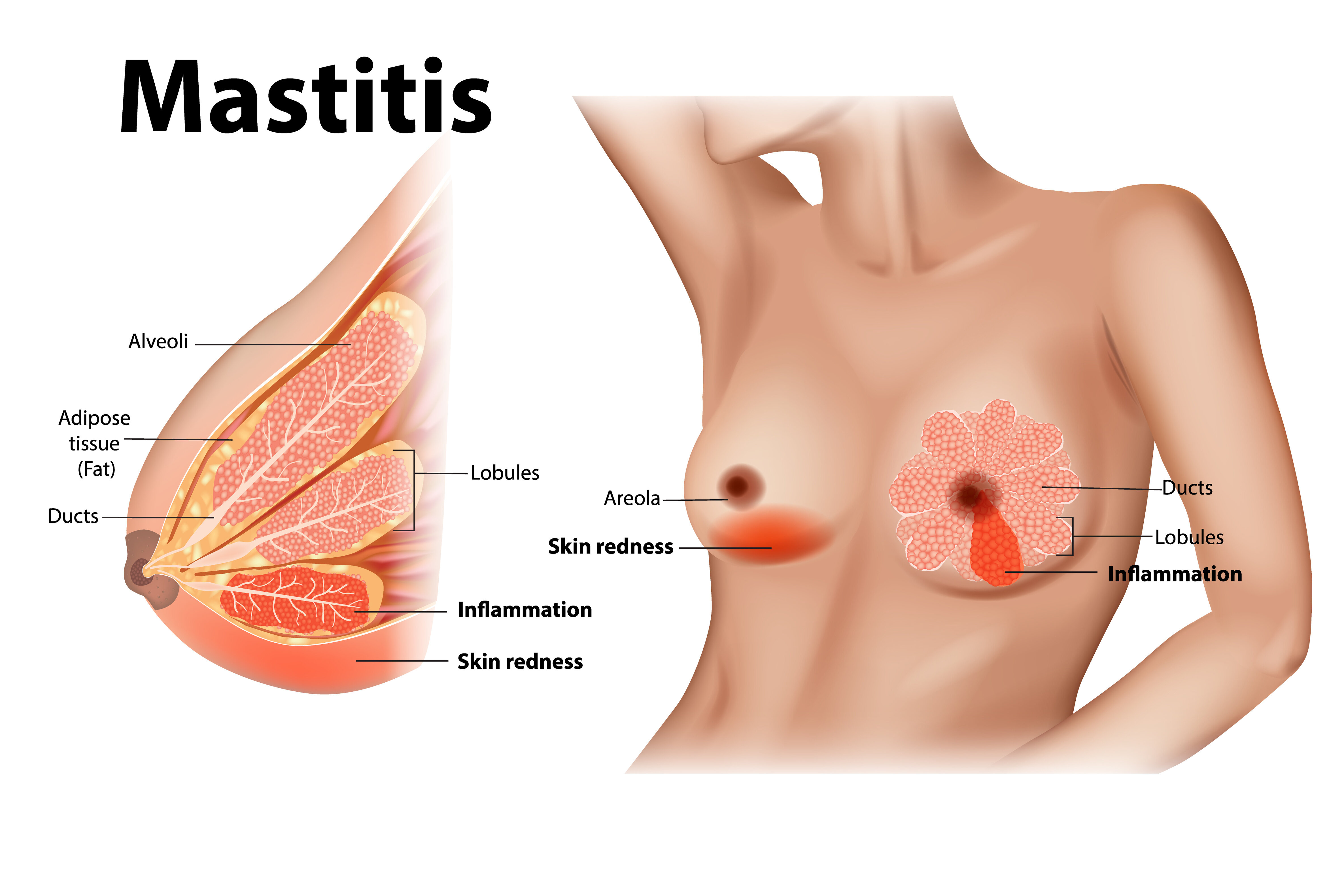
Mastitis is a painful inflammation of the breast tissue that usually occurs during breastfeeding—although it’s also possible for women who don’t breastfeed to develop a breast infection. Most breastfeeding women who are affected show symptoms during the first three months of breastfeeding. It’s important to remember that mastitis usually affects only one breast at a time.
What does mastitis look and feel like?
The early signs of mastitis resemble those of blocked milk ducts. The breast is swollen, painful and may feel slightly hot. Sometimes, the skin covering the affected area becomes red or takes on a darker colour. You may even feel one or several hard lumps in your breast or notice white or yellowish discharge coming out of your nipples.
In addition to these local symptoms, mastitis causes an overall feeling of discomfort that can include fever. In fact, it’s quite adequate to compare mastitis to having the flu, referring to the feeling of weakness, chills, aching limbs and general fatigue that are commonly associated with influenza.
The appearance of systemic symptoms is what distinguishes mastitis from blocked milk ducts. In the case of clogged ducts, symptoms only show in the affected area of the breast and don’t radiate out.
The most important mastitis symptoms at a glance:
- Localised symptoms: swelling, redness, lump(s), soreness, hotness of the skin, pain during feedings
- Systemic symptoms of inflammation: fever, malaise, fatigue, achings
What causes mastitis?
There are two main reasons why breast tissue gets inflamed, either blocked milk ducts or a bacterial infection. Medical professionals therefore distinguish between two types of breast inflammation: infectious (caused by bacteria) and non-infectious (caused by breast milk build-up) mastitis.
The underlying causes for non-infectious mastitis include:
- Incorrect breastfeeding position
- Poor latch
- Weak suck
- Oversupply of breast milk
- Irregular feedings
- External pressure that compresses the breast tissue
Causes for infectious mastitis include:
- Sore nipples that lead to open wounds and rhagades on and around the nipple, which provides an entry point for bacteria and other germs
- Poor hand hygiene through which bacteria and germs are transferred onto the breast
Factors that can further increase the risk of mastitis include excessive stress, smoking, nipple injuries (e. g. piercings) and weakness of the immune system.

How to treat mastitis?
Mastitis is a severe breast condition, which is why you should definitely talk to your midwife or lactation consultant to get professional advice on how to treat it.
But in the meantime, you can start with these practical tips:
- Cold therapy with the help of breast gel pads or cold compresses to relieve pain
- Use of painkillers that are safe to take while breastfeeding (e. g. paracetamol or ibuprofen)
- Rest and relaxation
- Gentle breast massage to stimulate milk flow
- Avoid wearing tight clothing
- Drinking plenty of fluids
The most important thing to do, however, is to continue breastfeeding—or express your milk by hand or with a breast pump. Regular emptying of your breast is the only way to relieve the pressure that builds up when your breasts get overly full.
How long does mastitis last?
Ideally, the symptoms should get better no later than 24 hours after you started treatment—48 hours when you need to take antibiotics. However, the complete healing process can take up to 14 days. It’s important to remember that the earlier you catch the signs of mastitis, the easier and quicker you can treat it and the better the chances that the symptoms will go away quickly.
How to prevent mastitis?
As a famous saying goes, prevention is better than cure. But how to prevent mastitis? Here are a few helpful tips you can follow in your daily breastfeeding routine.
- Make sure your baby latches on correctly
- Change your breastfeeding position often so that the breast gets emptied completely
- Don’t wait too long until the next feeding
- Use silver nursing cups to prevent sore nipples that can lead to infection
- Pay careful attention to hand hygiene to keep bacteria and germs away
- Avoid stress and take regular breaks
- Use warm compresses to stimulate milk flow and prevent engorgement
- Only wear well-fitting nursing bras
- Avoid pumping more milk than your baby needs
Mastitis vs. clogged milk ducts: What’s the difference?
Clogged milk ducts and mastitis lead to very similar symptoms, which can make it hard for breastfeeding mothers to tell them apart. Not to forget that blocked milk ducts can develop into mastitis if left untreated. So, how can you tell the difference between the two breast conditions to know when it’s time to go and see a doctor.
When suffering from clogged milk ducts, women usually only show localised symptoms such as breast pain, redness and swelling. If these localised symptoms appear in combination with systemic symptoms like fever, fatigue and a general feeling of discomfort, this typically indicates that the blockage in the milk ducts has progressed to mastitis.
Consistent treatment (breast massages, hot therapy, regular changing of breastfeeding position etc.) should lead to an improvement within 24 hours. If that’s not the case or if the symptoms get worse, it’s likely you are no longer suffering from blocked milk ducts but from mastitis. However, only a doctor can make a definite diagnosis.
Will mastitis go away on its own?
One thing’s for sure, mastitis is a severe health condition that shouldn’t be ignored. It causes more than just a little discomfort for the breastfeeding mum and definitely needs treatment. Untreated, mastitis can lead to a breast abscess which should be avoided at all costs. So, the answer to the question of whether mastitis will go away on its own is a clear no.
Can I still breastfeed with mastitis?
Unless you suffer from excruciating pain, you should try to continue breastfeeding. Your breasts still need to be emptied in order to prevent the formation of a breast abscess. Plus, regular breastfeeding will help improve your symptoms. You might have heard that breastfeeding with mastitis is unhealthy for the baby, but that’s a myth. As long as the pain is tolerable, you can and should keep breastfeeding.
When to seek professional help to treat mastitis?
If you are unsure about how to proceed or simply need some reassurance, you can always reach out to your midwife or contact a lactation consultant. Professional support is available from many different institutions and organisations so that getting the help you need is usually not a problem. In addition to providing guidance on how to cure mastitis, they can also help you find out what has caused your mastitis to prevent it from recurring.
If, after 24 or 48 hours, your symptoms don’t get better (or even get worse), you should consult a doctor who can prescribe antibiotics. Don’t hesitate to seek professional help straight away if both your breasts are affected or if you discover pus or blood in your breast milk.
References
- Mastitis and Sore Breasts - La Leche League International (llli.org)
- Mastitis: symptoms and treatment | Baby & toddler, Feeding articles & support | NCT
- Mastitis - La Leche League GB
- Mastitis, Slowed Milk Flow, and Milk Blisters - La Leche League USA (lllusa.org)
- Mastitis - HealthyChildren.org
- Your Guide to Breastfeeding (uncfsu.edu)
- Mastitis: Causes, Symptoms, Treatment & Prevention (clevelandclinic.org)
- Mastitis | Breastfeeding Challenges | Start for Life (www.nhs.uk)
- Mastitis and Breast Abscess: Symptoms and Treatment | Patient
















